Facts about Corneal Diseases
| Treatment Methods: | Visual aids, corneal transplants |
|---|---|
| Types of Corneal Diseases: | Corneal dystrophies (anterior, stromal, and posterior dystrophies), most common dystrophy: Fuchs’ endothelial dystrophy; corneal inflammations (keratitis) |
| Treatment Duration: | Depends on the chosen treatment method |
| Anesthesia: | Local anesthetic eye drops |
| Clinic Stay: | Outpatient |
| Aftercare: | Depends on the chosen treatment method |

Keratoconus
Keratoconus refers to a cone-shaped irregular protrusion of the cornea. This occurs because the cornea becomes thinner in its central parts due to reduced biomechanical stability in keratoconus. In the thinned areas, it bulges more under the intraocular pressure than in the (normally) thicker peripheral parts, resulting in a cone-shaped contour. Keratoconus occurs with a frequency of approximately 1:2000 in Central Europe.
Diagnosis is made, among other methods, by topographic or tomographic imaging (measurement of the corneal surface) using computer-assisted devices such as the Pentacam® HR.
Treatment
Rigid contact lenses are used to improve visual acuity. If rigid ("hard") contact lenses are not tolerated, in some cases so-called “intracorneal ring segments” (Intacs®, Keraring®) can be implanted using a femtosecond laser (Visumax®, Victus®) to improve vision.
If the disease shows progressive changes (increasing deformation of the cornea), the corneal surface can be treated with “Corneal Crosslinking.”
Corneal Crosslinking
Corneal Crosslinking strengthens the cornea by applying riboflavin (vitamin B2) drops and irradiating with UV-A light. The main applications are ectatic corneal diseases such as keratoconus or ectasia after refractive surgery (e.g., post-LASIK ectasia). Thanks to the latest technologies (Avedro KXL®), this treatment now only takes about 15 minutes and is performed under painless topical anesthesia with eye drops.
Corneal Dystrophies
Corneal dystrophies usually occur in both eyes, are hereditary, and show progression over time. They can be classified into anterior, stromal, and posterior dystrophies. The most common dystrophies include keratoconus and Fuchs’ endothelial dystrophy. In the latter, depending on the stage, a lamellar corneal transplant is usually necessary (DMEK).
Treatment
Corneal Transplantations:
DMEK

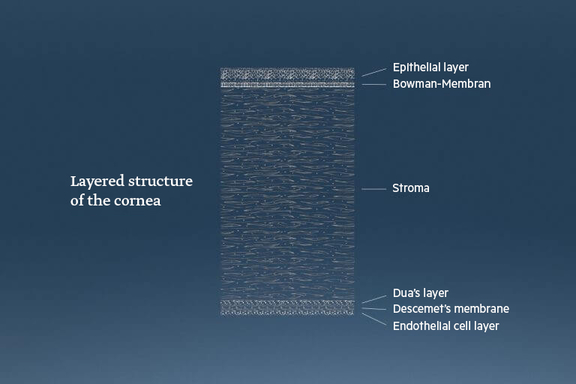
DMEK (Descemet Membrane Endothelial Keratoplasty) is the most advanced and least invasive type of corneal transplantation. In this procedure, only the innermost layer of the cornea (Descemet’s membrane and endothelium) is transplanted. The surgery can be performed under local anesthesia and no stitches are required. The main indications are Fuchs’ endothelial dystrophy or bullous keratopathy. Dr. Martin Dirisamer has already performed more than 200 of these operations and is recognized worldwide as a leading expert in this field.
(Femtosecond laser) DALK
Femtolaser-DALK (Deep Anterior Lamellar Keratoplasty) is a type of “deep anterior lamellar keratoplasty” further developed by Prof. Priglinger and Dr. Martin Dirisamer. The “FalKe” (Femtosecond Laser-Assisted Deep Anterior Lamellar Keratoplasty) treatment combines state-of-the-art laser technologies (Zeiss® VisuMax, Bausch & Lomb® Victus) with established methods (Melles dissection, Anwar’s Big Bubble technique). This allows for the treatment of various pathologies of the anterior corneal layers, such as advanced keratoconus, corneal scars from foreign bodies or infections, congenital corneal dystrophies, and more.
(Femtosecond laser) Penetrating keratoplasty
Penetrating keratoplasty has been successfully performed for over 100 years. In this procedure, all layers of the cornea are transplanted and temporarily fixed with sutures. As the standard method, mechanical trephine systems were used to cut the cornea in both the donor tissue and the recipient. In 2014, Dr. Martin Dirisamer and Prof. Priglinger presented the world’s first series of femtosecond laser-assisted penetrating keratoplasties using the Victus® laser (Bausch & Lomb®) in London. This OCT (optical coherence tomography)-controlled, micrometer-precise treatment is primarily intended to improve visual performance for the patient.
Corneal Inflammations (Keratitis)
Corneal inflammations can have a wide variety of causes. They are classified into chemical causes (corrosions), physical causes (UV exposure, “flash burns” during welding), mechanical causes (foreign bodies), genetic, neurological, and biological causes (bacteria, viruses, fungi, amoebae).
The course of keratitis can vary depending on the cause and severity, ranging from complete healing without consequences to the need for a corneal transplant.
Treatment
Corneal transplants:
- (Femtosecond laser) DALK (Deep Anterior Lamellar Keratoplasty)
- (Femtosecond laser) penetrating keratoplasty
The cornea – the unsung hero
When looking at the cornea compared to the entire eyeball, it appears rather inconspicuous and only a small part of the eye. But appearances are deceiving, because our cornea does a lot and makes a very important contribution to our clear vision. With a refractive power of +43 diopters (D), it carries the main part of the light refraction needed for image focusing (the eye as a whole has a refractive power of about 60 D).
What exactly is the cornea?
The cornea is the outermost front part of the eye and part of the outer eye coat. It is constantly moistened and nourished by tears produced by our eyelids and tear glands and is normally crystal clear. Also called the "window of the eye," it is a round disc separated from the sclera (the white of the eye). It consists of several layers, with the stroma making up about 90% of the cornea. Only in 2013 was the Dua’s layer—a very thin, just 15 µm thick but very strong membrane—discovered between the stroma and Descemet’s membrane.
Refractive power -/+
The cornea is actually thinner in its center (about 0.52 mm) than at the edge (about 0.67 mm), so it would basically act like a concave lens (diverging lens). However, because of the aqueous humor located behind it in the anterior chamber, it achieves the high positive refractive power (+43 D). When the horizontal and vertical radii are unevenly shaped, this condition is called astigmatism (corneal curvature irregularity).
Corneal metabolism
Our cornea depends heavily on external factors for constant supply of nutrients and oxygen. The tear film (especially oxygen) supplies the outer part, while the aqueous humor supplies the inner part (mainly nutrients). Only at the very edge is the so-called limbal vascular network located, which can supply the extreme edge of the cornea directly with glucose (sugar) and oxygen. The supply and breakdown of glucose is important and, if disturbed, can lead to clouding of the cornea.
Corrections of diseased cornea
Congenital or acquired refractive errors (such as astigmatism) can be corrected to some extent by refractive surgery (e.g., SMILE or Femto LASIK). The thickness and stability of the cornea are crucial here. High refractive errors can be corrected with artificial toric lenses. In this case, the cornea itself is not ablated, but the refractive behavior is influenced by the corresponding curvature of the artificial lens.
Other corneal dystrophies can now also be treated well. A common corneal anomaly is keratoconus, a cone-shaped protrusion due to thinning of the cornea that leads to severe refractive errors.
If it is such a corneal disease, a corneal transplant is possible. Here, the diseased tissue is replaced by suitable donor material, or a healthy corneal disc is sewn onto the patient’s cornea.
Conclusion
The cornea is an important part of our eye and our vision. By maintaining a healthy diet and sufficient fluid intake, we can create a good basis for the cornea to remain in shape for a long time and be adequately supplied with nutrients and oxygen. If problems or changes occur in the cornea, or in cases of congenital corneal anomalies, good treatment options are now available.
Frequently Asked Questions about Corneal Diseases
What is the purpose of the cornea in the eye?
The cornea, also called the cornea, is the transparent front part of the outer layer of the eye. It is gently curved and located at the front of the eyeball, allowing light to enter the eye. Together with the lens, it is responsible for the majority of the eye’s light refraction. Since the cornea is nearly as tough as horn substance, it is called the “horny” (horn-like) layer, or cornea.
Is it possible to see without a cornea?
Together with the eye lens, the cornea forms the optical system of the eye. What we see is only sharply focused on the retina if the cornea is evenly curved and also clear.
What are corneal diseases?
When the cornea is unevenly curved or cloudy, it leads to impaired vision and, in some cases, to what is called corneal blindness.
Is regeneration of the cornea in the eye possible?
No, the main component of the corneal tissue (called the corneal stroma) cannot regenerate itself. Therefore, injuries, diseases, infections, degenerative processes, or inherited malformations can cause scarring or clouding of the cornea. This can lead to impaired vision or even blindness.
How can you recognize a corneal disease?
Over time, a corneal disease becomes noticeable through visual impairments. Some corneal diseases cannot be detected in the early stages and progress very slowly. A clouding of the cornea can be identified by increased sensitivity to glare and a decrease in visual acuity. In some corneal diseases, symptoms are more pronounced in the morning upon waking and improve throughout the day. However, visual strain caused by dry eyes from activities like computer work or reading worsens the symptoms. Keratoconus first manifests as frequent changes in eyeglass prescription. Additionally, so-called dysphotopsias (streaks, double vision, and star-shaped rays) can occur.
What types of corneal diseases are there?
Basically, one distinguishes between corneal inflammations (keratitis), corneal injuries, corneal ulcers (ulcus corneae), corneal scars, corneal degeneration, corneal dystrophy (genetically caused), and an irregular curvature called keratoconus.
How is corneal dystrophy managed?
The treatment method for corneal dystrophies depends on the specific type of disease present. Nowadays, many cases can be treated surgically through laser treatment of the affected corneal tissue (e.g., phototherapeutic keratectomy; PTK) or by corneal transplantation (so-called keratoplasty; e.g., DMEK).
CONTACT
Ophthalmology Clinic Linz
Weissenwolffstraße 13, 3rd Floor
4020 Linz
Office Hours
Phone Consultation Hours
MON, WED, THU 09:00 AM – 6:00 PM
TUE 09:00 AM - 4:00 PM
FRI 09:00 AM – 12:00 PM
Appointment Days
By appointment only
Ophthalmology Clinic Vienna
Habsburgergasse 10, 4th Floor
1010 Vienna







