Facts about Macular Diseases
| Treatment Method: | Intravitreal Operative Medication Application (IVOM) |
|---|---|
| Symptoms: | Straight lines appear distorted, disappearing, dancing or distorted letters while reading, inability to recognize faces, persistent gray spot in front of the eye |
| Treatment Duration: | Less than 5 minutes |
| Anesthesia: | Locally anesthetic eye drops |
| Clinic Stay: | Outpatient |
| Aftercare: | Rest, avoid rubbing the eyes |

The term macular degeneration summarizes diseases that affect the "point of sharpest vision," the macula lutea. During the progression of macular disease, central vision deteriorates. This condition usually occurs in older age.
Macular disease can have two different causes. On one hand, deposits and degenerative processes can occur in the retina – this form is called dry macular degeneration. On the other hand, fluid accumulation in the retina can alter the structure of the macula. This condition is the most common and also the most serious form of age-related macular degeneration (AMD).
If fluid accumulates in the macula, it is called macular edema or wet macular degeneration. Poorly controlled and long-standing type 1 or type 2 diabetes can be among the causes. This is referred to as “diabetic macular edema.” As the disease progresses, it can lead to loss of reading ability.
Patients report the following complaints
Reading:
- Straight lines appear distorted
- Letters disappear while reading
- Letters “dance”
- Letters appear warped
Everyday life:
- Faces cannot be recognized
- Constant gray spot in front of the eye
Other conditions:
There are also diseases in which the macula develops a hole. If the so-called macular hole progresses, vision can slowly deteriorate, potentially resulting in loss of reading ability.
Another condition is the macular pucker. Here, a thin membrane grows over the macula, the area of sharpest vision. This condition, also called epiretinal gliosis, can likewise impair vision, causing reading ability to gradually decline as the disease progresses.
Diseases of the macula can be diagnosed, evaluated, and monitored by the ophthalmologist using a microscope called a slit lamp and supported by OCT measurement (optical coherence tomography).
Amsler grid test
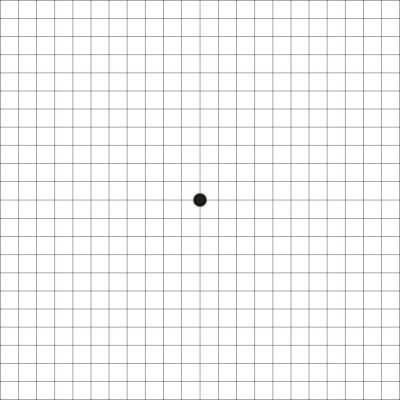
For self-monitoring, patients are advised to regularly perform the Amsler grid test. If patients wear reading glasses, the test should be done with the reading glasses on. The test is done with one eye at a time. The patient should fixate on the dot in the center and assess the grid surrounding the dot.
If any of the following complaints occur, the eyes should be checked by an eye specialist:
- Black spot in the center is not recognized
- Grid lines appear distorted
- Squares are uneven in size
- Dark spots in the grid
- Bright spots or “holes” in the grid
If a macular disease is known, the Amsler test should be performed regularly to detect any changes as early as possible.
Treatment
When letters “dance” or disappear while reading, lines appear distorted, and faces can no longer be recognized well because of gray spots in the field of vision, patients should promptly visit an ophthalmologist to check for possible macular degeneration (macula = center of the sharpest vision on the retina) or another macula-related disease (e.g., macular edema). Using a slit lamp, microscope, and macular OCT measurement, the type of macular degeneration can be determined.
AMD
Most patients who visit the ophthalmologist with these symptoms are older. Hence, this form is called Age-Related Macular Degeneration (AMD).
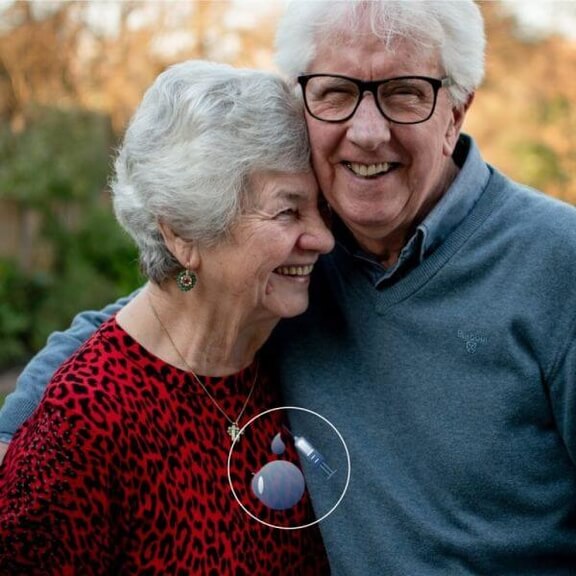
When the macula is affected, many patients are initially distressed by the diagnosis, but not all AMD conditions are an immediate threat to vision nowadays. IVOM therapy offers improvement.
IVOM treatment
IVOM stands for Intravitreal Operative Medication Application. It is a medication delivered directly into the eye via a specialized injection to act directly at the site. The most commonly used drugs to reduce macular edema are Avastin®, Lucentis®, Eylea®, or Ozurdex®.
These medications are VEGF inhibitors (Vascular Endothelial Growth Factor), which prevent uncontrolled growth of blood vessels in the eye. Excessive blood vessels can cause blood and fluid to accumulate on the retina, obstructing vision. Existing edema can no longer grow with therapy and is “dried out.”
Course of treatment
The VEGF inhibitor is injected directly into the eye. The treatment is outpatient; patients come to the practice and are prepared with a cleansing solution and local anesthesia. During the treatment, the eye is gently held open with a lid speculum. The procedure itself takes only a few minutes. After a short recovery phase, patients can leave the practice soon afterward.
Typically, patients need ongoing and regular therapy to stabilize the disease’s progression long-term. Usually, monthly check-ups and retreatments are scheduled at the beginning of therapy.
Great success
Until a few years ago, the course of this disease was difficult to influence. Today, depending on the condition, it is possible not only to stabilize the disease but in many cases to achieve noticeable improvements in vision for the patient. The treatment success rate is very high, giving many patients a significant increase in quality of life and personal independence
Frequently Asked Questions About Macular Degeneration
What is the macula?
The eyeball is lined on the inside with a thin layer of nerve cells called the retina. At the center of this layer is the macula, the central part of the retina, which is only a few millimeters in size. It is a small spot where the focused light of the perceived image is concentrated and transmitted as an electrical impulse to the brain. In this tiny area, about 6 million photoreceptor cells (so-called cones), responsible for color vision and the central sharpness of our eyes, are concentrated. Any change to the macula can affect central vision in such a way that you may perceive dark spots in your field of vision or see things distorted.
What is age-related macular degeneration (AMD)?
Age-related macular degeneration refers to changes in the macula that affect central vision and become more common with increasing age. There are two forms of degeneration affecting the cone cells: dry AMD and wet AMD. While dry AMD progresses slowly, wet AMD leads to irreversible damage to central vision and loss of reading ability within a relatively short time. Therefore, in the case of wet AMD, it is important to treat damage caused by fluid accumulation in the tissue early on. Medications can be used to reduce the fluid buildup in the layers of the macula. Wet macular degeneration can only be slowed down; a cure is not currently possible.
What is meant by an intravitreal injection (IVOM)?
An intravitreal operative medication application, abbreviated as IVOM, is especially used when fluid accumulation in the layers of the macula needs to be treated in cases of wet macular degeneration, or when the formation of new, harmful blood vessels needs to be halted.
During the treatment, specific drugs are introduced into the eye using a microscopically fine syringe. The eyes are numbed with drops beforehand, so the injection is usually painless for the patient. The IVOM medications suppress the formation of new blood vessels, thereby preventing the progression of AMD (age-related macular degeneration) or DME (diabetic macular edema). Since the inhibitors only work for a limited period, multiple injections are necessary.
What are the prospects of success in the treatment of macular degeneration?
The treatment of wet macular degeneration has been almost revolutionized by so-called anti-VEGF medications: thanks to intravitreal injections with drugs such as Eylea, Lucentis, and Avastin, which aim to reduce fluid accumulation in the layers of the macula, the visual prognosis for most patients can be significantly improved. However, since these inhibitors only work for a limited time—because the drug concentration in the eye decreases after a while, leading to fluid buildup in the macula—they need to be injected multiple times. The goal of these treatments is long-term stabilization of AMD (age-related macular degeneration). A complete cure, however, is still not possible to date.
Is the recurrence of wet macular degeneration possible?
In most cases, it is possible to suppress the newly formed blood vessels (so-called choroidal neovascularizations) through intravitreal operative medication administration (IVOM therapy). However, this does not automatically address the underlying cause of the development of new blood vessels. If the therapy is stopped too early, the neovascularizations often reoccur. Therefore, it is especially important to choose a continuous, long-term treatment for AMD (age-related macular degeneration).
What risks are associated with IVOM treatment?
IVOM therapy is extremely low-risk. By far the most common side effect is a small red blood spot at the injection site (so-called hyposphagma), which is harmless and usually disappears on its own within about a week. Possible complications also include retinal detachments or bleeding into the vitreous body. However, the risk of these complications is very low, with a probability well below 1%.
What should be considered after the treatment?
After the injection, the eyes are often very sensitive, which may cause increased itching and a sensation of a foreign body. This is harmless and can be relieved with eye drops, which you can obtain at the pharmacy. Usually, these symptoms disappear within one day at the latest. Small spots may also appear in your field of vision, but there is no cause for concern, as these are usually tiny gas bubbles contained in the medication that dissolve on their own. In rare cases, mild and harmless conjunctival hemorrhages may occur, which disappear after a few days. If you experience prolonged pain, severe redness, or distorted vision, please contact us.
CONTACT
Ophthalmology Clinic Linz
Weissenwolffstraße 13, 3rd Floor
4020 Linz
Office Hours
Phone Consultation Hours
MON, WED, THU 09:00 AM – 6:00 PM
TUE 09:00 AM - 4:00 PM
FRI 09:00 AM – 12:00 PM
Appointment Days
By appointment only
Ophthalmology Clinic Vienna
Habsburgergasse 10, 4th Floor
1010 Vienna







